https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5594987/
Common causes of upper GI bleeding: peptic ulcer disease (62%), arteriovenous malformations (10%), gastritis or duodenitis (8%) and esophageal varices (6%)
Common causes of lower GI bleeding: diverticular disease (40%), colitis and inflammatory bowel disease (21%), neoplasia (14%), coagulopathic hemorrhage (12%) and angiodysplasia
Diagnostic Modalities
Upper endoscopy and colonoscopy
- First-line diagnostic and therapeutic modality
- 98% sensitivity, 100% specificity
- Allows for direct visualization of the mucosa to identify the source of bleeding, enable application of hemostatic therapy and can be used for tissue sampling in cases of suspected malignancy
Radionucleotide Imaging
- Performed with technetium-99m tagged red blood cells
- High sensitivity; capable of detecting rates of bleeding as low as 0.05–0.1 ml min
- Not ideal for clinically unstable patients
- Cannot provide precise anatomic localization of the site of active bleeding
Catheter Angiography
- First-line imaging and treatment modality for patients who are unstable with lower GI bleeding, patients following a failed upper or lower endoscopy and patients with lower GI bleeding with a source of bleeding visualized on an additional imaging modality
- Can detect rates of bleeding as low as 0.5 ml/min and has the added major advantage of allowing for treatment of GI bleeding.
- Invasive and time-consuming procedure with a potentially high radiation dose
Multi-Detector CT Angiography
- Ideal initial diagnostic test for patients who are hemodynamically stable with acute GI bleeding, as well as for patients awaiting catheter angiography or endoscopy
- Sensitivity of 97% and specificity of 100% using arterial and portal venous phase images.
- CTA has the advantage of being able to precisely localize the source of arterial and venous GI bleeding, and to diagnose underlying pathology that may be the cause of bleeding to direct future management
- CTA can uniquely diagnose causes of GI bleeding that are not within the GI tract, such as haemobilia
- Lower sensitivity than radionucleotide imaging, and false-negative results can occur if the patient is not bleeding at the time of the scan
TLDR:

Diagnostic algorithm for UGIB

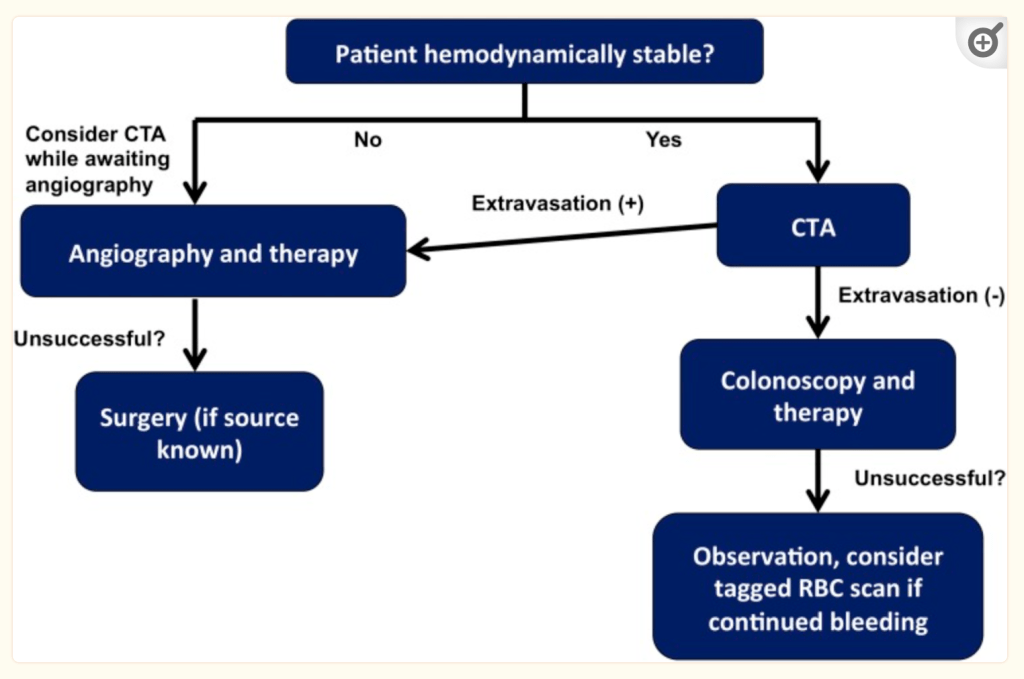
Diagnostic algorithm for LGIB
Leave a comment